What is Translational Medicine?
Translational medicine is an interdisciplinary process relating to the transition of biomedical discoveries into real-world treatments for patients and impacts on community health. This process spans discovery-based science, the lab bench, implementation, the bedside, and the community, and combines expertise and disciplines from all of these areas. The overall goal of translational medicine is to improve healthcare by enhancing and accelerating prevention, diagnosis and therapeutic applications.
The Translational Medicine Pipeline
Translational medicine is often divided into five stages, T0-T4, each representing different parts of the research pipeline from discovery to the community. We believe that through the Academy of Translational Medicine, we can have a direct and significant impact on the timeline, costs and success rate in the T0-T2 stages of the translational medicine process. In addition, by more actively engaging patients, care providers, health systems, policy makers, regulatory, and industry experts in the earliest stages of the translational process (T0-T2), we believe that the ATM can also indirectly but significantly impact the number, quality and cost of products that reach T3 and T4.

Stages of the Translational Pipeline
Example
T0: Basic and Applied Research
Discovering a new compound for treating hepatitis C, and using cell culture and animal models to ensure the safety of the compound in animals and that the target is actionable.
T1: Translation to Humans
Testing that the new compound is safe in healthy humans
T2: Translation to Patients
Testing that the new compound is safe and efficacious in hepatitis C patients compared to current care.
T3: Translation to Practice
Developing screening programs to identify hepatitis C patients that will benefit the most from the new treatment and finding strategies for providing timely care to those patients.
T4: Translation to the Community
Studying if the new hepatitis C treatment prevents the development of serious hepatitis C-related complications like liver cancer, thereby improving the patient’s quality of life and ability to work, while freeing up resources for the healthcare system.
Why do we need the Academy of Translational Medicine?
We are entering a golden age of biomedical discovery and innovation, where new classes of therapeutics — such as mRNA, gene, and cell therapies — devices, and diagnostics have the potential to transform patient care for many diseases, where treatment options are limited or non-existent. However, concerns about the rising cost of new therapeutics is a key issue for health system sustainability. Making the process of developing new therapeutics, devices and diagnostics more efficient will help address both access and affordability.
 In 2020, the UBC Faculty of Medicine established the Academy of Translational Medicine based on our belief that translating biomedical discoveries from bench to bedside takes too long and costs too much money. We looked at the incredible assets in B.C.’s bio-innovation ecosystem and recognized that the province has many of the building blocks in place for a complete end-to-end translational pipeline, which could enable local researchers to move more quickly and efficiently through the process of translating a new discovery into real-world impact for patients.
In 2020, the UBC Faculty of Medicine established the Academy of Translational Medicine based on our belief that translating biomedical discoveries from bench to bedside takes too long and costs too much money. We looked at the incredible assets in B.C.’s bio-innovation ecosystem and recognized that the province has many of the building blocks in place for a complete end-to-end translational pipeline, which could enable local researchers to move more quickly and efficiently through the process of translating a new discovery into real-world impact for patients.
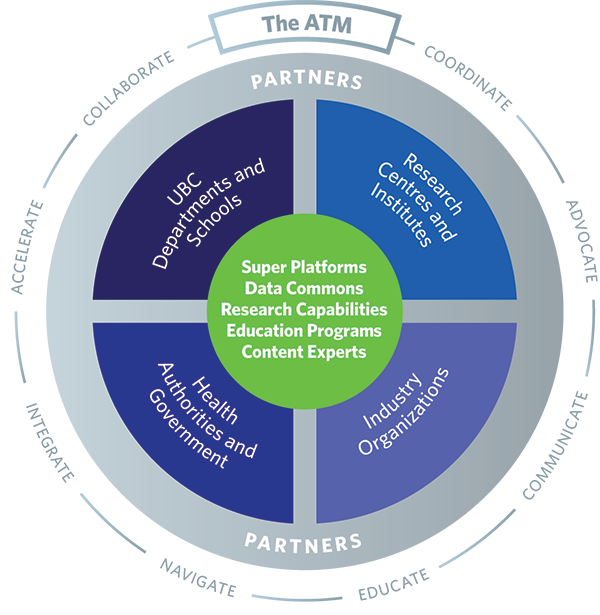
The Academy of Translational Medicine is an umbrella structure that connects these assets and fosters collaboration and innovation to support a wide range of outstanding translational research institutes, centres, and programs affiliated with UBC and our partners. It is a distributive model that aims to accentuate the many translational medicine strengths that already exist within the UBC ecosystem.
Our mission is to create a smoother, shorter path for biomedical translation that ensures faster access to the best possible therapies, devices, and diagnostics, providing the foundation for a more equitable, sustainable, and effective health care system for the future.